High blood pressure
Highlights
Blood Pressure Measurements
Blood pressure is measured in millimeters of mercury (mm Hg). The higher number indicates the systolic blood pressure, the pressure in your arteries while your heart is pumping blood. The lower number is the diastolic blood pressure, the pressure when your heart is relaxing and refilling with blood between beats. For adults:
- Normal blood pressure readings are below 120/80 mm Hg.
- High blood pressure (hypertension) is generally considered to be a blood pressure reading greater than or equal to 140 mm Hg (systolic) or greater than or equal to 90 mm Hg (diastolic).
- Blood pressure readings in the prehypertension category (120 -139 systolic or 80 - 89 diastolic) indicate an increased risk for developing hypertension.
- A blood pressure reading of 139/89 mm Hg or below should be the minimum goal for everyone. People with heart disease, peripheral artery disease, diabetes, or chronic kidney disease should strive for 130/80 or less. Blood pressure goals are being reexamined for African-Americans and for people with diabetes and chronic kidney disease.
Blood Pressure Screening Guidelines
- Current guidelines from the U.S. Preventive Services Task Force recommend that all adults age 18 years and older have their blood pressure measured.
- People with high blood pressure should be screened for diabetes. The U.S. Preventive Services Task Force recommends that all patients with blood readings of 135/80 mm Hg or higher be screened for type 2 diabetes. (The American Diabetes Association recommends screening for patients with blood pressure greater than 140/90.)
Home Blood Pressure Monitoring
Most patients with high blood pressure will benefit from monitoring their blood pressure at home on a regular basis. Home monitoring can help show if blood pressure medications are working or if they need to be adjusted.
Lifestyle Changes and High Blood Pressure
Lifestyle changes are important for preventing and treating high blood pressure. Healthy changes include maintaining a normal weight, exercising regularly, quitting smoking, limiting alcohol consumption to no more than one or two drinks a day, reducing sodium (salt) intake, and increasing potassium intake. The DASH diet is a diet plan proven to help improve blood pressure.
Medications for High Blood Pressure
Drug treatment for high blood pressure is tailored to the individual patient. There are many different types of blood pressure medications. Although some patients need only one drug to control blood pressure, the most recent guidelines from the American College of Cardiology and the American Heart Association recommend a combination of two or more medications for patients with blood pressure above 140/90 mm Hg.
Blood pressure measurements can fluctuate throughout the day and in different environments. The decision to start or increase blood pressure medications should not be based on a single blood pressure reading. To obtain the most accurate estimate of your true blood pressure, your doctor will use an average of multiple readings. These may include repeated readings made in the doctor’s office as well as blood pressure measurements you performed at home.
Introduction
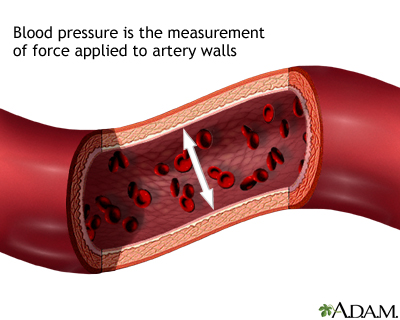
High blood pressure, also called hypertension, is elevated pressure of the blood in the arteries. Hypertension results from two major factors, which can be present independently or together:
- The heart pumps blood with excessive force.
- The body's smaller blood vessels (known as the arterioles) narrow, so that blood flow exerts more pressure against the vessels' walls.
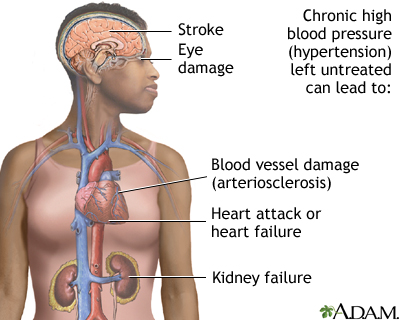
Although the body can tolerate increased blood pressure for months and even years, eventually the heart may enlarge (a condition called hypertrophy), which is a major factor in heart failure.
Such pressure can also injure blood vessels in the heart, kidneys, the brain, and the eyes.
Two numbers are used to describe blood pressure: the systolic pressure (the higher and first number) and the diastolic pressure (the lower and second number). Health dangers from blood pressure may vary among different age groups and depending on whether systolic or diastolic pressure (or both) is elevated. A third measurement, pulse pressure, may also be important as an indicator of severity.
Systolic Blood Pressure. The systolic pressure (the first and higher number) is the force that blood exerts on the artery walls as the heart contracts to pump out the blood. High systolic pressure is a greater risk factor than diastolic pressure for brain, heart, kidney, and circulatory complications and for death, particularly in middle-aged and elderly adults.
Diastolic Blood Pressure. The diastolic pressure (the second and lower number) is the measurement of force as the heart relaxes to allow the blood to flow into the heart. High diastolic pressure is a strong predictor of heart attack and stroke in young adults.
Pulse Pressure. Pulse pressure is the difference between the systolic and the diastolic readings. It indicates stiffness and inflammation in the blood-vessel walls. The greater the difference between systolic and diastolic numbers, the greater the risk to health.
Hypertension Categories
There are a number of ways to categorize or describe hypertension.
- Primary Hypertension. Primary hypertension, also called essential or idiopathic hypertension, is high blood pressure without a known cause. About 90% of all high blood pressure cases are this type.
- Secondary Hypertension. Secondary hypertension is hypertension caused by another underlying medical condition, such as kidney or endocrine disorders. It comprises about 5% of high blood pressure cases.
Other doctors categorize hypertension based on what portion of the blood pressure reading is abnormal:
- Isolated Systolic Hypertension. Elevated systolic pressure can pose a significant danger for heart problems and stroke even when diastolic is normal -- a condition called isolated systolic hypertension. This occurs when systolic pressure is over 140 mm Hg but diastolic pressure is under 90 mm Hg. It is related to arteriosclerosis (hardening of the arteries). Isolated systolic hypertension is the most common form of hypertension in people older than age 50.
- Diastolic Hypertension. Diastolic hypertension refers to an elevated diastolic blood pressure reading (over 89 mm Hg). This subtype is most common in people age 30 - 50.
Blood Pressure Guidelines
Blood pressure is measured in millimeters of mercury (mm Hg). According to current adult guidelines, blood pressure is categorized as normal, prehypertensive, and hypertensive (which is further divided into Stage 1 and 2, according to severity).
- Normal blood pressure is below 120/80 mm Hg.
- Prehypertension blood pressure readings (120 -139 systolic or 80 - 89 diastolic) indicate an increased risk for developing high blood pressure.
- High blood pressure is greater than or equal to 140 mm Hg (systolic) or greater than or equal to 90 mm Hg (diastolic).
Current guidelines for children are based on percentile ranges for a child’s body size. Hypertension in children is defined as average systolic and diastolic readings that are greater than the 95th percentile for gender, age, and height on at least three occasions.
Prehypertension in children is diagnosed when average systolic or diastolic blood pressure levels are at least in the 90th percentile but less than the 95th percentile. For adolescents, as with adults, blood pressure readings greater than 120/80 are considered prehypertensive. Increasing rates of childhood obesity have led to higher rates of hypertension and prehypertension among children and adolescents.
Blood Pressure Ranges | |
Blood Pressure Category | Ranges for Most Adults (systolic/diastolic) |
Normal Blood Pressure (systolic/diastolic) | Systolic below 120 mm Hg Diastolic below 80 mm Hg |
Prehypertension | Systolic 120 - 139 mm Hg Diastolic 80 - 89 mm Hg (NOTE: 139/89 or below should be the minimum goal for everyone. People with heart disease, peripheral artery disease, diabetes or chronic kidney disease should strive for 130/80 or less. Blood pressure goals are being reexamined for African-Americans and for people with diabetes and chronic kidney disease.) |
Mild Hypertension (Stage 1) | Systolic 140 - 159 mm Hg Diastolic 90 - 99 mm Hg |
Moderate-to-Severe Hypertension (Stage 2) | Systolic over 160 mm Hg or Diastolic over 100 mm Hg |
Note: If one of the measurements is in a higher category than the other, the higher measurement is usually used to determine the stage. For example, if systolic pressure is 165 (Stage 2) and diastolic is 92 (Stage 1), the patient would still be diagnosed with Stage 2 hypertension. A high systolic pressure compared to a normal or low diastolic pressure should be a major focus of concern in most adults. | |
Causes
Causes of Primary Hypertension
Hypertension is referred to as essential (primary) when the doctor is unable to identify a specific cause. It is by far the most common type of high blood pressure. The causes of this type, while unknown, are likely to be a complex combination of genetic, environmental, and other factors. [For risk factors of developing primary hypertension, see the Risk Factors section of this report.]
Genetic Factors. A number of genetic factors or interactions between genes play a major role in essential hypertension. Genes under investigation include:
- Genes that regulate a group of hormones known collectively as the angiotensin-renin-aldosterone system. This system influences all aspects of blood pressure control, including blood vessel contraction, sodium and water balance, and cell development in the heart.
- Genes that cause abnormalities of the sympathetic nervous system. This is the part of the autonomic nervous system that controls heart rate, blood pressure, and the diameter of the blood vessels.
Causes of Secondary Hypertension
Secondary hypertension is caused by an underlying medical condition or other factor (such as medications) that elevates blood pressure. Many different medical conditions are associated with secondary hypertension. These conditions can also make high blood pressure more difficult to control.
Diabetes. Hypertension is strongly associated with diabetes, both type 1 and type 2. Kidney damage (diabetic nephropathy) is generally the cause of high blood pressure in people with diabetes.
Kidney Disease. Kidney disease is the most common cause of secondary hypertension, particularly in older people. In addition to diabetic nephropathy, many other types of kidney diseases can cause hypertension. Renal artery stenosis involves the narrowing of the renal artery and is usually caused by atherosclerosis. Other types of kidney disease associated with hypertension are polycystic kidney disease and renal parenchymal disease.
Coarctation of the Aorta. Coarctation of the aorta is a birth defect that causes narrowing of the aorta, the main artery of the heart.
Endocrine Disorders. Adrenal tumors (pheochromocytoma, aldosteronism), thyroid disorders, and Cushing syndrome can all cause secondary hypertension.
Medications. Many different prescription and over-the-counter drugs can temporarily raise blood pressure or worsen existing high blood pressure. They include:
- Corticosteroids when given by mouth or intravenously
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin, generic), naproxen (Aleve, generic), and aspirin
- Cold medicine decongestants containing pseudoephedrine can increase blood pressure in people with high blood pressure, although they appear to pose no danger for those with normal blood pressure.
- Oral contraceptives (birth control pills) increase the risk for high blood pressure, particularly in women who are older than 35 years, obese, smokers, have strong family history of hypertension, or some combination of these factors. Stopping the pill nearly always reduces blood pressure.
Risk Factors
In the United States, about 1 in 3 adults has high blood pressure. Many people with high blood pressure are unaware that they have it.
About 30% of American adults have prehypertension. People who are diagnosed with prehypertension (blood pressure ranges from 120 - 139/80 - 89 mm Hg) are at increased risk of developing high blood pressure.
Age and Gender
Age is the major risk factor of hypertension. Men over age 45 and women over age 55 are at increased risk for high blood pressure. Over half of Americans over age 60 have hypertension. After age 65, high blood pressure affects more women than men. Hypertension is also becoming more common in children and teenagers. Among younger people, boys are at higher risk for high blood pressure than girls.
Race and Ethnicity
Compared to Caucasians and other ethnic groups, African-Americans are much more likely to have high blood pressure. More than 40% of African-American men and women have hypertension. (African-American women have a higher risk than African-American men.) High blood pressure tends to start at a younger age among African-Americans, is often more severe, and causes greater risks for premature death from heart attack, stroke, heart failure, and kidney failure.
Family History
People with parents or other close relatives who have high blood pressure have an increased risk of developing it themselves.
Obesity
About a third of patients with high blood pressure are overweight. Even moderately obese adults have double the risk of hypertension than people with normal weights. Children and adolescents who are obese are at increased risk for high blood pressure when they reach adulthood.
Obstructive Sleep Apnea
Obstructive sleep apnea, a disorder in which breathing halts briefly but repeatedly during sleep, is present in many patients with hypertension. The relationship between sleep apnea and hypertension has been thought to be largely due to obesity, but studies are finding a higher rate of hypertension in people with sleep apnea regardless of their weight.
Lifestyle Factors
Smoking. Cigarette smoking is a major risk factor for high blood pressure.
Sodium (Salt) and Potassium. Eating too much sodium (salt) can increase the risk for developing high blood pressure. Similarly, a diet that is too low in potassium can make the body accumulate too much sodium. Sodium and potassium are important regulators of fluid balance in cells.
Alcohol. Chronic heavy alcohol use can increase blood pressure. Women may be more sensitive than men to the blood pressure effects of alcohol.
Physical Inactivity. A sedentary lifestyle and lack of physical activity can increase the risk of becoming overweight.
Stress. Mental and emotional stress can cause a temporary increase in blood pressure. Chronic stress can lead to engaging in unhealthy behaviors (overeating, smoking, alcohol use, lack of exercise) that contribute to high blood pressure.
Symptoms
High blood pressure is often called the "silent killer" because it usually produces no symptoms until vital organs like the heart, brain, and kidneys are damaged. Hypertension increases slowly over the years. Everyone 18 years and older should have their blood pressure measured on a regular basis. It is particularly important for anyone with risk factors to have their blood pressure checked regularly and to make appropriate lifestyle changes. Such recommendations are especially important for people who have prehypertension or hypertension, a family history of hypertension, are overweight, or are over age 40.
Symptoms of Malignant Hypertension
In rare cases (fewer than 1% of all patients with hypertension), the blood pressure rises quickly (with diastolic pressure usually rising to 130 mm Hg or higher), resulting in malignant or accelerated hypertension. This is a life-threatening condition and must be treated immediately. People with uncontrolled hypertension or a history of heart failure are at increased risk for this crisis.
People should call a doctor immediately if these symptoms occur:
- Drowsiness
- Confusion
- Headache
- Nausea
- Loss of vision
- Respiratory distress (difficulty breathing)
Diagnosis
Most physical exams include a blood pressure reading. Patients should not smoke, exercise, or drink caffeinated beverages within 30 minutes before their blood pressure measurement.
Measuring Blood Pressure
- The standard instrument used to measure blood pressure is called a sphygmomanometer. Measurements are given as units of mercury, which for many years was used to fill the central column in standard sphygmomanometers. (Modern devices do not use mercury.)
- An inflatable cuff with a meter attached is placed around the patient's arm over the artery while the patient is seated, their back is supported, and the arm being used is around the level of the heart. The inflated cuff briefly interrupts the flow of blood in the artery, which then resumes as the cuff is slowly deflated.
- The person taking the blood pressure listens through a stethoscope.
- The first pumping sound is recorded as the systolic pressure, and the last sound is the diastolic pressure.
- If a first blood pressure reading is above normal, the health professional may take two or more measurements separated by 2 minutes with the patient sitting or lying down. Another measurement may be taken after the patient has been standing for 2 minutes. If the measurements are still elevated, your health care provider should take blood pressure readings from both arms.
- Decisions on starting or increasing medications should be based on multiple blood pressure readings, including both those taken at the doctor’s office and at home.

Although this test has been used for more than 90 years, it is not completely accurate or sensitive. The following factors can cause a falsely low pressure reading:
- An arm cuff that is too wide
- Dehydration
Falsely high pressure can result from:
- An arm cuff that is too small
- Stress
- Recently consuming foods or beverages (such as coffee) that raise blood pressure
- Recent tobacco exposure
- Recent exercise
Office blood pressure readings taken by a doctor are more likely to be higher than readings measured at home. This can be due to "white coat hypertension," which is blood pressure that is only elevated during a doctor's office visit. Patients with white coat hypertension have high readings in the office but a daytime blood pressure reading away from the doctor's office of less than 135/85 mg Hg and no evidence of complications of blood pressure elsewhere in the body. Patients with white-coat hypertension may require additional blood pressure monitoring.
Ambulatory Monitoring
Doctors may ask some patients to use a special ambulatory monitoring device for a 24-hour period. The device checks blood pressure about every 15 - 30 minutes during the day and night and provides a read-out of blood pressure measurements for the doctor. Ambulatory monitoring may be used for patients who have borderline high blood pressure or for those who have had difficulty keeping their blood pressure under control. It can also help distinguish between true and white-coat hypertension and it can detect so-called masked hypertension (readings that are normal in a doctor's office but high during daily life). Ambulatory monitoring can also be helpful for diagnosing children with suspected high blood pressure.
Home Monitoring
The American Heart Association (AHA) recommends that all patients with high blood pressure monitor their blood pressure at home on a regular basis. In addition to other benefits, home monitoring can help show if blood pressure medications are working.
The AHA recommends:
- Purchase a blood pressure monitor with cuffs that fit on the upper arm. Wrist monitors are not recommended. Make sure that the cuff is the right size (one size does not fit all).
- Ask your doctor to show you the proper way to use the monitor. Your arm should be supported, with the upper arm at heart level and feet on floor (back supported, legs uncrossed).
- Take two or three readings at a sitting, 1 minute apart, while resting in a seated position. It is important to take the readings at the same time each day, such as morning and night. Your doctor may suggest what specific times readings should be taken.
- The target goal of a reading is under 135/85 mm Hg or less than 130/80 mm Hg in high-risk patients.
Blood Pressure Variations at Home. In general, everyone's blood pressure varies in the same way throughout a given day. In monitoring at home, it is important to note these changes:
- Blood pressure is usually highest from morning to mid-afternoon.
- It normally dips to its lowest level during sleep. Some people (particularly postmenopausal women) have a condition called nondipper hypertension, in which blood pressure does not fall at night.
- Upon waking, blood pressure in most people typically increases suddenly. Early morning is the highest risk period for heart attack and stroke.
Physical Examination for Complications of Hypertension
If blood pressure is elevated, the doctor will check the patient's pulse rate, examine the back of the eye, examine the neck for distended veins or an enlarged thyroid gland, check the heart for enlargement and murmurs, and examine the abdomen and check the leg pulses.
Medical History
If hypertension is suspected, the doctor should obtain the following information:
- A family and personal medical history, especially relating to high blood pressure, stroke, heart problems, kidney disease, or diabetes.
- Risk factors for heart disease and stroke, including tobacco use, salt intake, obesity, physical inactivity, and unhealthy cholesterol levels.
- Any medications being taken.
- Any symptom that might indicate secondary hypertension (high blood pressure caused by another disorder). Such symptoms include headache, heart palpitations, excessive sweating, muscle cramps or weakness, or excessive urination.
- Any emotional or environmental factors that could affect blood pressure.
Laboratory and Other Tests
If a physical examination indicates hypertension, additional tests may help determine whether organ damage is present.
Blood Tests and Urinalysis. These tests are performed to check for a number of factors, including potassium levels, cholesterol, blood sugar (to screen for diabetes), infection, kidney function, and other possible problems. Measuring blood levels of the protein creatinine, for example, is important for all hypertensive patients in order to determine kidney damage.
Tests to Evaluate the Heart. These tests include:
- An electrocardiogram (ECG) is performed on most patients in the doctor's office.
- An exercise stress test may be needed for patients who also have symptoms of coronary artery disease.
- An echocardiogram is needed when it would help the doctor decide whether to start treatment. Most of the time this test is not necessary for patients who have only hypertension and no other symptoms.
Tests to Evaluate the Kidneys. These tests include:
- A Doppler or duplex test may be performed to see whether one of the arteries supplying blood to the kidney is narrowed, a condition called renal artery stenosis.
- An ultrasound may also be performed to examine the kidneys.
Complications
Hypertension places stress on several organs (called target organs), including the kidneys, eyes, and heart, causing them to deteriorate over time. High blood pressure contributes to 75% of all strokes and heart attacks. It is particularly deadly in African-Americans.
Other risk factors combined with significantly high blood pressure can increase the likelihood of complications. These risk factors include increasing age, smoking, abnormal cholesterol levels, family history of premature heart disease, obesity, diabetes, coronary artery disease, or other evidence of vascular disease.
Heart Complications
High blood pressure is a major risk factor for hypertensive heart disease, the leading cause of illness and death from high blood pressure. Hypertensive heart disease is a group of complications that include:
Coronary Artery Disease. High blood pressure contributes to the thickening of the blood vessel walls, which can cause or worsen atherosclerosis (accumulated deposits of cholesterol in the blood vessels). The end result is coronary artery disease (CAD), also called ischemic heart disease, which increases the risk for angina (chest pain), heart attack, stroke, and death. High blood pressure is the most common risk factor for heart attack and stroke.
Heart Failure. High blood pressure increases the heart's workload. Over time, this can cause the heart muscle to thicken. As the heart pumps against elevated pressure in the blood vessels, the left ventricle becomes enlarged and the amount of blood pumped by the heart each minute (cardiac output) goes down, a condition called left ventricular hypertrophy (LVH). Without treatment, this can lead to heart failure.
Cardiac Arrhythmias. High blood pressure increases the risk for cardiac arrhythmias (disturbances and irregularities in heartbeats). Arrhythmias include atrial fibrillation, premature ventricular contractions, and ventricular tachycardia.
Stroke
About two-thirds of people who suffer a first stroke have moderate elevated blood pressure (160/95 mm Hg or above). Hypertensive people have up to 10 times the normal risk of stroke, depending on the severity of the blood pressure in the presence of other risk factors. Hypertension is also an important cause of silent cerebral infarcts, which are blockages in the blood vessels in the brain (mini-strokes) that may predict major stroke or progress to dementia over time.
Diabetes and Kidney Disease
Diabetes. High blood pressure, and some of the medications used to treat it, can increase the risk for developing diabetes. There are strong biologic links between insulin resistance (with or without diabetes) and hypertension. It is unclear if one condition causes the other.
Current guidelines recommend that most people with diabetes or chronic kidney disease should reduce their blood pressure to 130/80 mm Hg or lower to protect the heart and help prevent other complications common to both diseases. Up to 75% of cardiovascular problems in people with diabetes may be due to hypertension.
The United States Preventive Services Task Force recommends screening for type 2 diabetes in all patients with blood pressure higher than 135/80 mm Hg.
End-Stage Kidney Disease. High blood pressure causes 30% of all cases of end-stage kidney disease (medically referred to as end-stage renal disease, or ESRD). Only diabetes leads to more cases of kidney failure. Patients with diabetes and hypertension need to be monitored very closely for the development of kidney disease.
Dementia
Isolated systolic hypertension may pose a particular risk for dementia (memory loss).
Eye Damage
High blood pressure can injure the blood vessels in the eye's retina, causing a condition called retinopathy.
Sexual Dysfunction
Sexual dysfunction is more common and more severe in men with hypertension and in smokers than it is in the general population. Although older drugs used to treat hypertension caused erectile dysfunction as a side effect, the disease process that causes hypertension is itself a major cause of erectile dysfunction. Oral phosphodiesterase type 5 (PDE5) inhibitors -- such as sildenafil (Viagra), tadalafil (Cialis), vardenafil (Levitra), and avanafil (Stendra) -- do not appear to pose a risk for most men who have both high blood pressure and erectile dysfunction. However, men who have uncontrolled or unstable hypertension should not take these medications. Men who take nitrate medications for heart disease cannot take erectile dysfunction pills.
Pregnancy and High Blood Pressure
Many women who are likely to develop hypertension when they are older have their first elevated blood pressure readings during pregnancy. Elevated blood pressure readings generally show up early in pregnancy, before 16 - 20 weeks. (This condition is different than preeclampsia, described just below.) These women often require antihypertensive medications during pregnancy and closer monitoring of themselves and the fetus. Continued hypertension after the pregnancy is also not uncommon.
Severe, sudden high blood pressure in pregnant women is one component of a condition called preeclampsia (also called toxemia) that can be very serious for both mother and child. Preeclampsia occurs in up to 10% of all pregnancies, usually in the third trimester of a first pregnancy, and resolves immediately after delivery. Other symptoms and signs of preeclampsia include protein in the urine, severe headaches, and swollen ankles.
The reduced supply of blood to the placenta can cause low birth weight and eye or brain damage in the fetus. Severe cases of preeclampsia can cause kidney damage, convulsion, and coma in the mother and can be lethal to both mother and child. Women at risk for preeclampsia (particularly those with existing hypertension) are monitored carefully for its presence. Both mother and fetus are monitored closely after a diagnosis. Blood pressure medications may be required. Delivery is the main cure for preeclampsia. In severe cases, the obstetrician will need to induce pre-term birth.
Treatment
Patients with hypertension should work with their doctors to set blood pressure goals based on individual risk factors. Risk factors for heart disease include family history of heart disease, smoking, unhealthy cholesterol and lipid levels, diabetes, and age over 60 years old.
Lifestyle changes are important for everyone, and patients should routinely monitor their blood pressure at home. The decision to start or increase blood pressure medications should not be based on a single blood pressure reading in the doctor’s office but on repeated readings. Your doctor may ask you for a list of your home blood pressure readings to help provide a more accurate estimate of your true blood pressure. Studies indicate that blood pressure may be needed to be checked as many as five or six times to give the best estimate.
Drug treatment needs to be planned on an individual basis. In some patients, a single-drug regimen can control mild-to-moderate hypertension, but the latest guidelines recommend combination therapy with two or more drugs if a patient’s blood pressure is above 140/90 mm Hg. Each drug has specific benefits, but their effects may vary depending on the individual patient.
Drug Treatment
The most effective anti-hypertensive medications fall into the following five categories:
- Diuretics rid the body of extra water and salt. Thiazide diuretics are usually the first-line treatment for high blood pressure.
- Beta blockers block the effects of adrenaline and ease the heart's pumping action.
- Angiotensin converting enzyme (ACE) inhibitors reduce the production of angiotensin, a chemical that causes arteries to narrow.
- Angiotensin-receptor blockers (ARBs) block the action of angiotensin.
- Calcium-channel blockers (CCBs) decrease the contractions of the heart and widen blood vessels.
Side Effects and Problems in Compliance. One of the most difficult issues that patients face is that the treatment may make them feel worse than the disease, which usually has no symptoms. Whatever the difficulties, compliance with a drug and lifestyle program is worth the effort. It is very important that patients discuss medication concerns with their doctors. If current blood pressure drugs are causing uncomfortable side effects, the doctor may adjust dosages or combinations.
Withdrawal from Anti-Hypertensive Medications. Patients whose blood pressure has been well-controlled and who are able to maintain a healthy lifestyle may be able to withdraw from medications. They should do so in a step-down manner (gradual reduction) and be monitored regularly. Stopping too quickly can have adverse effects, including serious effects on the heart. The highest success rates are more likely in those who lose weight and reduce sodium intake, in patients who have been treated with a single drug, and in those who have maintained lower systolic blood pressure during treatment. People over 75 years old may have more trouble than younger adults maintaining normal blood pressure after withdrawal.
Treatment of Resistant Hypertension
Some patients are unable to meet target blood pressure goals despite consistently following a treatment plan that includes three or more medications. Factors that contribute to resistant hypertension include older age (especially age 75 or older), high baseline blood pressure, and medical conditions such as obesity, sleep apnea, diabetes, and chronic kidney disease. Treating any underlying medical condition is important for helping control blood pressure. Patients should be sure to adhere to lifestyle changes [weight loss and dietary changes, particularly sodium (salt) restriction] and may require modifications to their drug regimens. Patients with severe resistant hypertension should consider seeking a consultation with a doctor who specializes in treating high blood pressure.
Treatment of Older Adults
High blood pressure is very common in older adults and can be challenging to control. Current guidelines recommend a blood pressure target goal of less than 140/90 mm Hg in people ages 65 - 79 years, and a systolic blood pressure between 140 - 145 mm Hg in people 80 years and older. In general, older adults usually have an elevated systolic blood pressure and a normal or low diastolic blood pressure, a condition known as isolated systolic hypertension.
Medications can be very effective for controlling high blood pressure in older adults, even in those over age 80. The choice of medications will depend in part on a patient’s history of other heart problems. Blood pressure drugs prescribed for older patients are generally started at the lowest dose and then gradually increased as necessary. As with all patients with high blood pressure, lifestyle changes are an essential component of treatment.
Older adults should have their blood pressure monitored on a regular basis. Blood pressure readings should be taken while in a standing position, as well as while seated.
Treatment of Children
Children with high blood pressure should first be treated with lifestyle changes, including weight reduction, increased physical activity, and diet modification. If blood pressure is not controlled with lifestyle changes, drug treatment may be required. Results of studies evaluating outcomes of children with hypertension suggest that early abnormalities, including enlarged heart and abnormalities in the kidney and eyes, may occur even in children with mild hypertension. Children and adolescents with hypertension should be monitored and evaluated for any early organ damage. Secondary hypertension (high blood pressure due to another disease or drug) is more common in children than adults.
Lifestyle Changes
Healthy lifestyle changes are an important first step for lowering blood pressure. Current guidelines recommend that people should:
- Exercise at least 30 minutes a day.
- Maintain normal weight.
- Reduce sodium (salt) intake.
- Increase potassium intake.
- Limit alcohol consumption to no more than one or two drinks a day.
- Consume a diet rich in fruits, vegetables, and low-fat dairy products while reducing total and saturated fat intake. (The DASH diet is one way of achieving such a dietary plan.)
- Quit smoking.
Restricting Sodium (Salt)
Some sodium (salt) is necessary for health, but the amount is vastly lower than that found in the average American diet. High salt intake is associated with high blood pressure. According to the American Heart Association, everyone should restrict their salt intake to less than 1,500 mg a day. This is particularly important for people over age 50, all African-Americans, and everyone with high blood pressure. Sodium restriction lowers blood pressure and also helps protect against heart failure and heart disease.
Some people (especially African-Americans, older adults, people with diabetes, overweight people, and people with a family history of hypertension) are “salt sensitive,” which means their blood pressure responds much more to salt than other people. People with salt sensitivity have a higher than average risk of developing high blood pressure as well as other heart problems
Salt substitutes, such as Nusalt and Mrs. Dash (which contain mixtures of potassium, sodium, and magnesium), are available, but they can be risky for people with kidney disease or those who take blood pressure medication that causes potassium retention.
Here are some tips to lower your salt and sodium intake:
- Look for foods that are labeled low-sodium, sodium-free, no salt added, or unsalted. Check the total sodium content on food labels. Be especially careful of canned, packaged, frozen, and processed foods. A nutritionist can teach you how to understand these labels.
- Don’t cook with salt or add salt to what you are eating. Try pepper, garlic, lemon, or other spices for flavor instead. Be careful of packaged spice blends as these often contain salt or salt products (like monosodium glutamate, MSG).
- Avoid processed meats (particularly cured meats, bacon, hot dogs, sausage, bologna, ham, and salami).
- Avoid foods that are naturally high in sodium, like anchovies, nuts, olives, pickles, sauerkraut, soy and Worcestershire sauces, tomato and other vegetable juices, and cheese.
- Take care when eating out. Stick to steamed, grilled, baked, boiled, and broiled foods with no added salt, sauce, or cheese.
- Use oil and vinegar, rather than bottled dressings, on salads.
- Eat fresh fruit or sorbet when having dessert.
Increasing Potassium
A potassium-rich diet may help to reduce blood pressure. For people without risks for potassium excess, potassium-rich foods that can help include bananas, oranges, pears, prunes, cantaloupes, tomatoes, dried peas and beans, nuts, potatoes, and avocados. For people without risk factors for excess potassium levels, the recommended daily intake of potassium is 3,500 mg a day.
Some patients may need to take potassium supplements. However, people who take medications that limit the kidney's ability to excrete potassium, such as ACE inhibitors, digoxin, or potassium-sparing diuretics, should not take potassium supplements and should be aware of excess potassium in their diet.
DASH Diet
The salt-restrictive DASH diet (Dietary Approaches to Stop Hypertension) is proven to help lower blood pressure, and may have additional benefits for preventing heart disease and stroke. Effects on blood pressure are sometimes seen within a few weeks. This diet is not only rich in important nutrients and fiber but also includes foods that contain far more potassium (4,700 mg/day), calcium (1,250 mg/day), and magnesium (500 mg/day) and much less sodium (salt) than the typical American diet.
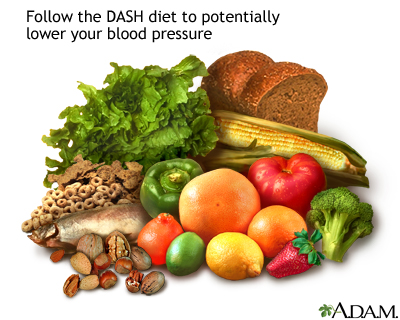
DASH diet recommendations:
- Limit sodium (salt) intake to no more than 2,300 mg a day (a maximum intake of 1,500 mg a day is now recommended by the American Heart Association).
- Reduce saturated fat to no more than 6% of daily calories and total fat to 27% of daily calories. (But, include dairy products that are non- or low-fat. Low-fat dairy products appear to be especially beneficial for lowering systolic blood pressure.)
- When choosing fats, select monounsaturated oils, such as olive or canola oils.
- Choose whole grains over white flour or pasta products.
- Choose fresh fruits and vegetables every day. Many of these foods are rich in potassium, fiber, or both, possibly helping lower blood pressure.
- Include nuts, seeds, or legumes (dried beans or peas) daily.
- Choose modest amounts of protein (no more than 18% of total daily calories). Fish, skinless poultry, and soy products are the best protein sources.
- Other daily nutrient goals in the DASH diet include limiting carbohydrates to 55% of daily calories and dietary cholesterol to 150 mg. Patients should try to get at least 30 g of daily fiber.
Other Dietary Considerations
Fiber. Increasing fiber in the diet may help reduce blood pressure levels.
Fish Oil and Omega 3 Fatty Acids. Omega 3 fatty acids (docosahexaenoic and eicosapentaneoic acids) are found in oily fish. Studies indicate that they may have specific benefits for many medical conditions, including heart disease and hypertension. They appear to help keep blood vessels flexible and may help protect the nervous system. Fatty acids are also available in supplements, but their long-term effects on blood pressure are unknown.
Calcium. Calcium regulates the tone of the smooth muscles lining blood vessels. Studies have found that people who have sufficient dietary calcium have lower blood pressure than those who do not. Hypertension itself increases calcium loss from the body. Results of studies evaluating the effects of extra calcium on blood pressure have been mixed, with some studies even showing higher pressure.
Weight Loss
Even modest weight loss in overweight people, particularly in the abdominal area, can immediately lower blood pressure. Weight loss, especially when accompanied by salt restriction, may allow patients with mild hypertension to safely reduce or go off medications. The benefits of weight loss on blood pressure are long-lasting.
Exercise
Regular exercise helps keep arteries elastic, even in older people, which in turn ensures blood flow and normal blood pressure. Doctors recommend at least 30 minutes of exercise on most days.
High-intensity exercise may not lower blood pressure as effectively as moderate intensity exercise and may be dangerous in people with hypertension. Older people and those with uncontrolled hypertension or other serious medical conditions should check with their doctors before starting an exercise program.
Good Sleep Habits
Certain sleep disorders, especially sleep apnea, are associated with hypertension. Even chronic, insufficient sleep may raise blood pressure in patients with hypertension, placing them at increased risk of heart disease and death. Stress hormone levels increase with sleeplessness, which can activate the sympathetic nervous system, a strong player in hypertension. Patients who have chronic insomnia or other severe sleep disturbances (particularly sleep apnea) may want to consult a doctor who specializes in sleep disorders. Patients with hypertension who are habitually poor sleepers should consider long-acting blood pressure medications to help counteract the increase in blood pressure that occurs in the early morning hours.
Stress Reduction
Stress reduction may help blood pressure control. Yoga, Tai chi, and relaxation techniques such as meditation may be beneficial.
Medications
Several classes of drugs are used to treat hypertension.
Diuretics
Diuretics help the kidneys get rid of excess salt and water. Thiazide diuretics are the mainstays of anti-hypertensive therapy and are often the first type of drug selected for most people with hypertension. They are also especially helpful for treating patients with heart failure, patients with isolated systolic hypertension, the elderly, and African-Americans. (African-Americans are more likely to be salt-sensitive, so they respond well to these drugs.) They also work well for patients with diabetes. Diuretics are often used in combination with other antihypertensive drugs.
There is strong evidence that diuretics work just as well as newer drugs in lowering blood pressure and are more effective in preventing heart failure, heart attack, and stroke.
Diuretic Types and Brands. The three main types of diuretics include:
- Thiazide diuretics. These include chlorothiazide (Diuril), chlorthalidone (Thalitone, Clorpres), indapamide (Lozol), hydrochlorothiazide (HydroDiuril), bendroflumethiazide (Naturetin), methylclothiazide, (Enduran), and metolazone (Zaroxolyn). All of these prescription drugs are available in generic form. In most cases, thiazides are preferred to other diuretics for treatment of high blood pressure. Some recent research favors chlorthalidone.
- Potassium-sparing diuretics. These include amiloride (Midamor, generic), spironolactone (Aldactone, generic), and triamterene (Dyrenium, generic).
- Loop diuretics. Because loop diuretics act faster than other diuretics it is important to avoid dehydration and potassium loss. Loop diuretics include bumetanide (Bumex, generic), furosemide (Lasix, generic), ethacrynic acid (Edecrin, generic), and torsemide (Demadex, generic).
Problems with Diuretics.
- Loop and thiazide diuretics reduce the body's supply of potassium, which, if left untreated, increases the risk for arrhythmias. Arrhythmias are heart rhythm disturbances that can, rarely, lead to cardiac arrest. If you experience reduced potassium, your doctor will prescribe a lower dose of the current diuretic, recommend potassium supplements, or switch to a potassium-sparing diuretic either alone or in combination with a thiazide.
- Potassium-sparing drugs have their own risks, which include dangerously high levels of potassium in people with existing elevated levels of potassium or in those with damaged kidneys. However, all diuretics are generally more beneficial than harmful.
- Thiazide diuretics may increase blood sugar levels.
- Erectile dysfunction (impotence) may be a side effect of thiazides.
- Elevated uric acid levels, and possibly gout, may be caused by thiazide diuretics.
Common Diuretic Side Effect Symptoms.
- Fatigue
- Depression and irritability
- Urinary incontinence
- Reduced sexual drive and problems with obtaining and maintaining an erection
Beta Blockers
Beta blockers help slow heart rate and lower blood pressure. They are usually used in combination with other drugs such as ACE inhibitors and diuretics. Beta blockers are more likely to be used to treat hypertension in patients with angina, previous heart attack, arrhythmias with fast heart rates, or migraine headaches. With careful use, they can be beneficial for patients with heart failure.
Brands. Propranolol (Inderal), acebutolol (Sectral), atenolol (Tenormin), betaxolol (Kerlone), carteolol (Cartrol), metoprolol (Lopressor), nadolol (Corgard), penbutolol (Levatol), pindolol (Visken), carvedilol (Coreg), timolol (Blocadren), and nebivolol (Bystolic). The drugs may differ in their effects and benefits. With the exception of nebivolol, all of these drugs are available in generic form.
Problems with Beta Blockers.
- Do not abruptly stop taking these drugs. The sudden withdrawal of beta blockers can rapidly increase heart rate and blood pressure and potentially cause angina or heart attack. If you need to stop your beta blocker, the doctor may want you to slowly decrease the dose before stopping completely.
- Beta blockers are categorized as non-selective or selective. Non-selective beta blockers, such as carvedilol and propranolol, may sometimes narrow bronchial airways. Patients with asthma, emphysema, or chronic bronchitis should not use these medicines.
- These drugs can hide warning signs of low blood sugar (hypoglycemia) in patients with diabetes. When combined with a diuretic, the risk of diabetes may increase.
- They may be less effective than other drugs for preventing stroke.
Common Side Effects.
- Fatigue and lethargy
- Vivid dreams and nightmares
- Depression
- Memory loss
- Dizziness and lightheadedness
- Reduced ability to exercise
- Coldness in extremities (legs, toes, arms, and hands)
- Reduced sexual drive and problems with obtaining and maintaining an erection
Check with your doctor about any side effects. Do not stop taking these drugs on your own.
ACE Inhibitors
Angiotensin-converting enzyme (ACE) inhibitors widen blood vessels and decrease the workload of the heart. They treat high blood pressure and can also help protect the heart and kidneys.
Patients with heart failure or an enlarged left ventricle, previous heart attack, diabetes, or kidney disease are considered particularly good candidates for ACE inhibitors as part of treatment for high blood pressure.
Aspirin is recommended for reducing the risk of cardiac problems in patients with heart disease, and can safely be used in combination with ACE inhibitors, particularly at lower dosages of aspirin (75 - 81 mg).
Brands. ACE inhibitors include captopril (Capoten, generic), enalapril (Vasotec, generic), quinapril (Accupril, generic), benazepril (Lotensin, generic), ramipril (Altace, generic), perindopril (Aceon, generic), and lisinopril (Prinivil, Zestril, generic).
Common Side Effects of ACE Inhibitors.
- Low blood pressure is the main side effect of ACE inhibitors. This can be severe in some patients, especially at the start of therapy.
- Irritating cough is a common side effect, which some people find intolerable.
- ACE inhibitors can harm a developing fetus and should not be used during pregnancy. Women who become pregnant should change from ACE inhibitors to another type of blood pressure drug as soon as possible. Women of child-bearing age who are considering becoming pregnant should also discuss other medications with their doctors.
- ACE inhibitors can increase potassium levels, particularly in patients with kidney disease.
Uncommon Side Effects of ACE Inhibitors.
- ACE inhibitors protect against kidney disease, but they may also increase potassium retention by the kidneys. If potassium levels become extremely high, they can cause the heart to stop beating (cardiac arrest). This side effect is uncommon, except in patients with significant kidney disease. Because of this risk, ACE inhibitors are not usually used in combination with potassium-sparing diuretics or potassium supplements.
- A rare but severe side effect is granulocytopenia, an extreme reduction in infection-fighting white blood cells.
- In very rare cases, patients suffer a sudden and severe allergic reaction, called angioedema that causes swelling in the eyes and mouth and may close off the throat.
Patients who have difficulty tolerating ACE inhibitor side effects are usually switched to an angiotensin-receptor blocker (ARB).
Angiotensin-Receptor Blockers (ARBs)
ARBs, also known as angiotensin II receptor antagonists, are similar to ACE inhibitors in their ability to widen blood vessels and lower blood pressure. They may have fewer or less-severe side effects than ACE inhibitors, especially coughing, and are sometimes prescribed as an alternative to ACE inhibitors. In general they are prescribed to patients who cannot tolerate or did not respond to ACE inhibitors.
Brands. Losartan (Cozaar, Hyzaar, generic), olmesartan (Benicar) candesartan (Atacand), telmisartan (Micardis), eprosartan (Teveten), irbesartan (Avapro), valsartan (Diovan), and azilsartan (Edarbi).
A combination medication containing candesartan and the diuretic hydrochlorothiazide (Diovan HCT, Atacand HCT) is also available. Exforge HCT is a triple-combination medication that combines in one pill valsartan along with the calcium-channel blocker amlodipine and the diuretic hydrochlorothiazide. Tribenzor combines in one pill olmesartan, amlodipine, and hydrochlorothiazide.
Side Effects.
- Low blood pressure
- Dizziness and lightheadedness
- Raised potassium levels
- Drowsiness
- Nasal congestion
- Should not be used during pregnancy
Calcium-Channel Blockers (CCBs)
Calcium-channel blockers (CCBs), also known as calcium antagonists, help relax blood vessels. Along with diuretics, CCBs may work better than other drug classes for lowering blood pressure in African-Americans. Recent research indicates that newer types of drugs (CCBs, ACE inhibitors) may be a better treatment option for some patients than older drugs (especially beta blockers).
Brands. Diltiazem (Cardizem, Dilacor), amlodipine (Norvasc), felodipine (Plendil), isradipine (DynaCirc), verapamil (Calan, Isoptin, Verelan), nisoldipine (Sular), nicardipine (Cardene), and nifedipine (Adalat, Procardia). All of these prescription medications are available as generics. For patients who have both high blood pressure and high cholesterol, Caduet combines in one pill amlodipine and the statin drug atorvastatin.
Side Effects.
- Swelling in the feet
- Constipation
- Fatigue
- Erectile dysfunction
- Gingivitis
- Rash
- Food interactions (do not take CCBs with grapefruit or Seville orange products)
Alpha Blockers
Alpha blockers such as doxazosin (Cardura, generic), prazosin (Minipress, generic), and terazosin (Hytrin, generic) help widen small blood vessels. They are generally not used as first-line drugs for high blood pressure, but are prescribed if other drugs do not work or as add-on medication.
Vasodilators
Vasodilators help open blood vessels by relaxing muscles in the blood vessel walls. These drugs are usually used in combination with a diuretic or a beta blocker. They are rarely used by themselves. Vasodilators include hydralazine (Apresoline, generic), clonidine (Catapres, generic), and Minoxidil (Loniten, generic). Some of these drugs should be used with caution or not at all in people who have angina or who have had a heart attack.
Other Drugs
Aliskiren (Tekturna). Aliskiren (Tekturna, Amturnide) is a new kind of antihypertensive drug called a direct renin inhibitor. It blocks renin, a kidney enzyme associated with high blood pressure. Aliskiren is also available in the 2-in-1 combination pills Tekturna HCT (aliskiren and the diuretic hydrochlorothiazide) and Tekamlo (aliskiren and the calcium channel blocker amlodipine). Aliskiren is prescribed either alone or in combination with other blood pressure medications. However, patients with diabetes or kidney impairment should not take aliskiren along with ACE inhibitors or ARBs because of increased risk for kidney damage and other problems. Aliskiren should not be used during pregnancy as it can cause injury or death to the fetus.
Resources
- www.acc.org -- American College of Cardiology
- www.heart.org-- American Heart Association
- www.ash-us.org -- American Society of Hypertension
- www.nhlbi.nih.gov/hbp -- National Heart, Lung, and Blood Institute
References
Adrogué HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007 May 10;356(19):1966-78.
AHA; ACC; National Heart, Lung, and Blood Institute, Smith SC Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol. 2006 May 16;47(10):2130-9.
Aronow WS, Fleg JL, Pepine CJ, Artinian NT, Bakris G, Brown AS, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011 May 17;57(20):2037-114. Epub 2011 Apr 26.
Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007 Nov 10;335(7627):974. Epub 2007 Nov 1.
Beulens JW, Rimm EB, Ascherio A, Spiegelman D, Hendriks HF, Mukamal KJ. Alcohol consumption and risk for coronary heart disease among men with hypertension. Ann Intern Med. 2007 Jan 2;146(1):10-9.
Blood Pressure Lowering Treatment Trialists' Collaboration, Turnbull F, Neal B, Ninomiya T, Algert C, Arima H, et al Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ. 2008 May 17;336(7653):1121-3. Epub 2008 May 14.
Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, et al. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med. 2010 Jan 25;170(2):126-35.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008 Jun 24;117(25):e510-26.
Cook NR, Obarzanek E, Cutler JA, Buring JE, Rexrode KM, Kumanyika SK, et al. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow-up study. Arch Intern Med. 2009 Jan 12;169(1):32-40.
Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007 Sep 25;116(13):1488-96. Epub 2007 Sep 10.
Drozda J Jr, Messer JV, Spertus J, Abramowitz B, Alexander K, Beam CT, et al. ACCF/AHA/AMA-PCPI 2011 Performance Measures for Adults With Coronary Artery Disease and Hypertension: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. Circulation. 2011 Jul 12;124(2):248-70. Epub 2011 Jun 13.
Ernst ME, Moser M. Use of diuretics in patients with hypertension. N Engl J Med. 2009 Nov 26;361(22):2153-64.
Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007 Nov;25(11):2193-8.
Flack JM, Sica DA, Bakris G, Brown AL, Ferdinand KC, Grimm RH Jr, et al. Management of high blood pressure in Blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010 Nov;56(5):780-800. Epub 2010 Oct 4.
Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009 Jul 22;302(4):401-11.
Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011 Feb;42(2):517-84. Epub 2010 Dec 2.
Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007 Aug 22;298(8):874-9.
Kaplan NM and Victor RG. Systemic hypertension: therapy. In: Bonow RO, Mann DL, Zipes DP, Libby P, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Saunders; 2012:chap 46.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009 May 19;338:b1665. doi: 10.1136/bmj.b1665.
Magnussen EB, Vatten LJ, Lund-Nilsen TI, Salvesen KA, Davey Smith G, Romundstad PR. Prepregnancy cardiovascular risk factors as predictors of pre-eclampsia: population based cohort study. BMJ. 2007 Nov 10;335(7627):978. Epub 2007 Nov 1.
Matchar DB, McCrory DC, Orlando LA, Patel MR, Patel UD, Patwardhan MB, et al. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers for treating essential hypertension. Ann Intern Med. 2008 Jan 1;148(1):16-29. Epub 2007 Nov 5.
Moser M, Feig PU. Fifty years of thiazide diuretic therapy for hypertension. Arch Intern Med. 2009 Nov 9;169(20):1851-6.
Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D; et al. Call to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008 Jul;52(1):10-29. Epub 2008 May 22.
Powers BJ, Olsen MK, Smith VA, Woolson RF, Bosworth HB, Oddone EZ. Measuring blood pressure for decision making and quality reporting: where and how many measures? Ann Intern Med. 2011 Jun 21;154(12):781-8, W-289-90.
Selassie A, Wagner CS, Laken ML, Ferguson ML, Ferdinand KC, Egan BM. Progression is accelerated from prehypertension to hypertension in blacks. Hypertension. 2011 Oct;58(4):579-87. Epub 2011 Sep 12.
Urbina E, Alpert B, Flynn J, Hayman L, Harshfield GA, Jacobson M, et al. Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008 Sep;52(3):433-51. Epub 2008 Aug 4.
U.S. Preventive Services Task Force. Screening for type 2 diabetes mellitus in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008 Jun 3;148(11):846-54.
Victor RG and Kaplan NM. Systemic hypertension: mechanisms and diagnosis. In: Bonow RO, Mann DL, Zipes DP, Libby P, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Saunders; 2012:chap 45.
Wolff T, Miller T. Evidence for the reaffirmation of the U.S. Preventive Services Task Force recommendation on screening for high blood pressure. Ann Intern Med. 2007 Dec 4;147(11):787-91.
|
Review Date:
5/22/2012 Reviewed By: Harvey Simon, MD, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |















